occupational therapy
Stroke
S.C.I. (Spinal Cord Injury)
Head Injury
G.B.S. (Guillain-Barre Syndrome)
Parkinson Disease
Autism
C.P. (Cerebral Palsy)
Down Syndrome
A.D.H.D. (Attention-Deficit Hyperactivity Disorder)
Intellectual Disability
Hand Therapy
Mental Health
Inclusive School
C.B.R. (Community Based Rehabilitation)
Ergonomics
Splinting & Assistive Device
Stroke

According to WHO 1982, “Stroke is a rapidly developed clinical signs of focal (or global) disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent cause other than vascular origin’’.
***If the disturbance resolve spontaneously within 24 hours is called Transient Ischemic Attacks (TIA).
WARNING SYMPTOMS:
Warning signs may last a few moments and then disappear. They are signs of a serious condition.
- Sudden weakness or numbness of the face, arm or leg on one side of the body
- Sudden dimness or loss of vision, particularly in one eye
- Sudden difficulty in speaking or trouble in understanding speech
- Sudden severe headache with no known cause
- Unexplained dizziness, unsteadiness, or sudden falls
COMPLICATION:
-
- Sensory disturbance
- Abnormal patterns of movement
- Abnormal Muscle tone
- Presence of Associated reaction
- Emotional Disturbance
- Speech & Language Disorder
- Visual Disturbance
- Perceptual Deficits
- Others
• Dysphagia
• Hemiplegic gait
HOW OCCUPATIONAL THERAPY CAN HELP?
When dealing with strokes, occupational therapists work through the usual occupational therapy processes:
- Ax and Training of sensory motor functions.
- Ax and training of cognitive functions (Memory retraining, Problem solving).
- Ax and training of Activity of Daily Living (ADL) skills-
- (Dressing retraining, Washing retraining, eating retraining, etc.).
- Advice and instruction in the use of adaptive devices.
- (Wheelchair, elbow crutch, parallel bar, etc.)
- Provision of splints and slings (cock up splint, resting splint, etc.)
- Education of family and primary caregivers with MDT.
- Psychological Counselling (Depression, Relationship issues, etc.).
- Facilitation of safe discharge.
- Impact of communication on engagement.
- Environmental Modifications
-
-
- This would include house modifications, ramps or rails that may be required
-
- Referral to support agencies, vocational services.
S.C.I. (Spinal Cord Injury)
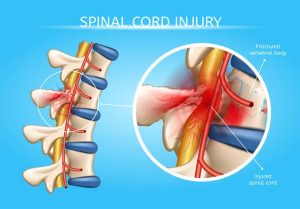
Spinal Cord Injury
- An injury to the vertebral column can result in an injury to the spinal cord which can affect all of its functions below the level of injury.
- Spinal Cord Injury (SCI) is an insult to the spinal cord resulting in a change, either temporary or permanent, in its normal motor, sensory, or autonomic function.
International Standard for Neurological Classification of Spinal Cord Injury (ISNCSCI)
Causes of SCI
- Traumatic
- Motor Vehicular Accident (Leading cause globally), fall from height (Second leading cause globally), Violence – Bullet / Stab Injury, Fall of Load from height, Diving Accident, Sports Injury.
- Non traumatic
Congenital- Spinal dysraphism, Amold-chiari malformations, Skeletal malformations, Other congenital
Genetic disorders- Hereditary spastc paraparesis, Spinino cerebellar ataxies, Adreno-myeloneurophies, other leukodystrophies, Spinal muscular atrophies, Genetic-other
Acquired abnormalities- Vertebral column degenerative disorders, Metabolic disorders, Vascular disorders, Inflammation auto immune disorders, Radiation related, Toxic, Neoplastic, Infection, Miscellaneous
How Occupational Therapy Can Help?
- Acute Phase
- Positioning, Splinting, Hand Therapy, Psychological Support, Pain management, Introduce Leisure activities, Career education
- Active Phase
- Functional bed mobility, Transferring, W/C mobility, Introduce functional activities, Splinting, Hand Therapy, Participation in art & song class.
- Rehab Phase
- Retraining ADLs, Advanced Transferring, Functional mobility, W/C Assessment & advanced W/C skills training, Prescribe assistive devices & modification,Vocational Assessment, Education
- Community reintegration Phase
- Work place & home environment modification, Career education & training, Social skills training, Engage ADL & DADL, Rickshaw transferring, Prepare Pt for WR, Home visit
Head Injury

The Brain Injury Association (BIA-2000) defines traumatic brain injury (TBI) as an insult to the brain, not degenerative or congenital, that is caused by an external force. This result may produce a diminished or altered state of consciousness and resultant impairment of cognitive, behavioural, emotional, or physical functioning.
Head Injury: A head injury can be defined as “damage to living brain tissue that is initially caused by external mechanical forces”. That excludes brain injury caused by internal events such as blood vessel rupture (stroke), tumours, viruses or development of disease.
Causes: Common causes of head injury include –
- Traffic accidents
- Fails
- Physical assault and
- Accidents at home, work, outdoors or while playing sports.
Classification: Head injury can be classified as–
- Closed head injury
- Open or penetrating head injury
Who suffers from Head Trauma?
- Head trauma can affect anyone at any age.
- Males, in between 15 and 24 years of age, are more vulnerable because of their high-risk lifestyles particularly from automobile accident and violent crime.
- Young children and individuals over 75 years of age are also more susceptible to head injury.
- Infants, toddlers, and elderly people can be affected by head injury after falling around the home.
- Violent shaking of an infant or toddler is another significant cause.
HOW OCCUPATIONAL THERAPY CAN HELP?
Following area should asses for head injured patient according to Occupational therapy point of view.
- Physical
Motor-
- Fine and gross motor skills
- Postural control and balance
- Range of motion and joint mobility
- Muscle tone
- Coordination
- Endurance
- Bilateral coordination
Sensory-
- Pain
- sensory awareness and discrimination
- Level of arousal
- Cognition and perception
- Daily living activities
- Psychosocial
- Social interaction skills
- Copping skills
- Learning skills
- Leisure interest and skills
G.B.S. (Guillain-Barre Syndrome)
GBS – is an acute autoimmune peripheral neuropathy involving patchy demyelination of the peripheral neurons.
Cause:
· GBS is typically preceded by an infection, either respiratory or gastrointestinal in nature.
· It is believed that the body’s antibodies (that are fighting the viral infection) mistake the myelin cells as infective cells and attack and destroy the myelin sheath.
· This influences the speed that neural impulses can travel to the neuromuscular junction, resulting in decreased muscle activation and weakness.
Diagnosis:
- Diagnosis is made through the use of nerve conduction studies, CSF analysis – (GBS has elevated levels of protein) and neurological examination – (asymmetrical weakness, absent reflexes)
HOW OCCUPATIONAL THERAPY CAN HELP?
When dealing with GBS, occupational therapists work through the usual occupational therapy processes:
Physical
- Postural control exercises
- Balance exercises
- During deterioration and plateau of condition, a maintenance program is needed involving ROM and stretching, oedema management, positioning and splinting (for positioning)
- During recovery phase incorporate a graded strengthening program as the natural recovery occurs
- Oedema Management – oedema can become a significant if the patient is ventilated
- Encourage family involvement in the UL program
- Use of adaptive devices to enhance function (built up cutlery, universal cuff, overhead suspension slings)
- Provide education and promote awareness of sensory issues
ADLs
Promoting independence in ADL’s and improving activity tolerance is very important. Graded participation in ADL’s as natural recovery occurs in the following areas:
- Dressing retraining, Washing retraining, eating retraining, Cooking retraining etc.
- Also the use of aids and equipment (overhead suspension sling and universal cuff for independent feeding
Fatigue Management and Education
Environmental Modifications
- This would include house modifications, ramps or rails that may be required
Parkinson Disease
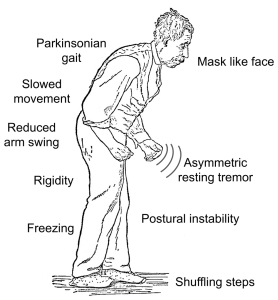
PD is a chronic, progressive, unremitting, and highly variable condition. PD is the 3rd most common neurological disease after CVA and Alzheimer’s Dementia. The incidence increases with age, with initial onset usually occurring between the ages of 45 and 75 years. PD is widespread in all ethnic groups and is more common in men with a male to female ratio of 3:2.
The cause of PD is idiopathic (unknown).
Signs and Symptoms
Tremor, Rigidity, Bradykinesia, Postural instability, Gait disorders, Dementia, Depression, Insomnia, Urinary frequency and urgency, Drooling, Speech disturbance, Difficulty in smelling.
HOW OCCUPATIONAL THERAPY CAN HELP?
- OT’s have a role in the management of PD from the onset to end stage and review by an OT at various stages throughout the disease is recommended.
- A detailed home assessment is seen as essential to the management of patient with PD.
- OT intervention with PD patients primarily involves the following therapy strategies
- Modifying the task
- Modifying the tools
- Modifying the environment
- Patient and carer education
Autism

Autism spectrum disorder (ASD) is a developmental disorder that affects communication and behavior. Although autism can be diagnosed at any age, it is said to be a “developmental disorder” because symptoms generally appear in the first three years of life.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a guide created by the American Psychiatric Association used to diagnose mental disorders, people with ASD have:
- Difficulty with communication and interaction with other people.
- Restricted interests and repetitive behaviors
- Symptoms that hurt the person’s ability to function properly in school, work, and other areas of life.
HOW OCCUPATIONAL THERAPY CAN HELP?
- Sensory integration therapy: Sensory integration therapy is provided as a part of or in addition to educational and behavioral programs.
- Behavioral therapy: It focuses on the child’s action, the parents are also required to learn different methods of coping with other children.
- Hand therapy: Fine motor delays are also common among children with autism. Fine motor delays impacts a person in areas including: hand writing, dressing oneself, brushing own teeth’s and feeding own self. Occupational therapist worked for it. They use different fine motor activities.
- Daily life therapy: Trained teachers together with parents facilitate group activities and the children are put through intensive physical and functional activity (dressing, feeding, bathing etc.). This is carried out under a regimented schedule and aims to improve the child independence in daily life.
- Group therapy: Group work aims to enable the child to learn different methods of reacting situation, role play etc.
- Social skills training: This techniques is used to teach children and adults with autism how to interact socially.
- Music therapy: Children with autism often process music batter then they process speech and have accurate memory for the lyrics of songs, so the possible use of music therapy in autism intriguing.
C.P. (Cerebral Palsy)

Cerebral palsy is a disorder of movement, muscle tone or posture that is caused by an insult to the immature, developing brain, most often before birth.
Signs and symptoms appear during infancy or preschool years. In general, cerebral palsy causes impaired movement associated with exaggerated reflexes, floppiness or rigidity of the limbs and trunk, abnormal posture, involuntary movements, unsteadiness of walking, or some combination of these.
People with cerebral palsy may have difficulty with swallowing and commonly have eye muscle imbalance. People with cerebral palsy may have reduced range of motion at various joints of their bodies due to muscle stiffness.
Causes
´ Cerebral palsy is caused by an abnormality or disruption in brain development, usually before a child is born. In, the exact trigger of this abnormality isn’t known. Factors that may lead to problems with brain development include:
´ Maternal infections that affect the developing fetus.
´ Fetal stroke, a disruption of blood supply to the developing brain.
´ Lack of oxygen to the brain related to difficult labor or delivery. This is rarely a cause.
´ Infant infections that cause inflammation in or around the brain.
´ Traumatic head injury to an infant from a motor vehicle accident or fall.
Clinical features of CP
´ CP is frequently limp & floppy when the baby birth.
´ Slow development.
´ The baby cannot use his hand.
´ Feeding problems.
´ Communication problem.
´ Poor IQ level.
´ Sense of touch, pain, heat, cold sensation is loss.
´ Abnormal reflex.
´ Abnormal muscle tone.
´ Involuntary movement.
´ Motor developmental delay.
´ Child cannot walk cannot perform other activity.
´ Sensory impairment.
´ Poor feeding ability.
´ Hearing impairment.
´ Drooling of saliva.
´ Decreased ROM.
´ Sometime arise deformity.
HOW OCCUPATIONAL THERAPY CAN HELP?
Occupational therapy aimed at helping the child to achieve or maintain their maximum level of independent and to develop practical life skills so that the child can participate to his/her full potential in the home and classroom environment.
• Sensory Integration Therapy: Improves the ability to receive, register, interpret and act on information that comes to the brain through sensory receptors.
• Moving safely
• Sustaining posture e.g. sitting for table top activities
• Fine motor skills e.g. hand writing
• Gross motor skills e.g. moving from one position to another or balance skills
• Concentration/attention
• Organization, planning and sequencing
• Self-esteem and social skills
• Self-care skills such as feeding self or getting dressed
- Using alternative strategies and adaptive equipment, occupational therapists work to promote your child’s independent participation in daily activities and routines in the home, the school and the community.
- Adaptive equipment may include walkers, quadrupedal canes, seating systems or electric wheelchairs.
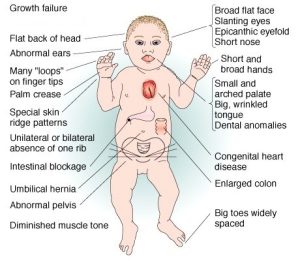
Down Syndrome

A set of physical, mental and behavioral characteristics that are due to a specific genetic abnormality (Leshin, 2003).It is a congenital disorder arising from a chromosome defect.
Cause:
Typically, the nucleus of each cell contains 23 pairs of chromosomes, half of which are inherited from each parent. Down syndrome occurs when an individual has a full or partial extra copy of chromosome 21
It’s known as trisomy 21. This additional genetic material alters the course of development and causes the characteristics associated with Down syndrome. Each person with Down syndrome is a unique individual and may possess these characteristics to different degrees, or not at all.
Sign & Symptoms
HOW OCCUPATIONAL THERAPY CAN HELP?
- The child with Down syndrome delays in gross motor skills, fine motor skills, cognitive skills, and communication.
- OT assesses all areas of development (Gross motor skill, fine motor skill, behavior, social skills, cognition and perception) for comprehensive management planning.
- OT may use different tests to assess Down syndrome child.
- OT checks following sensorimotor components-
Muscle tone, Muscle strength, Range of motion, Coordination and balance, Posture, Hand function.
- Cognitive and perceptual component it includes-
Attention, Memory, Figure-ground, Directionality
- Social components-
- Social smile
- Peer relationship
- Group interaction
- Behavior and Communication (verbal & non-verbal).
- Sensory Integration (SI) Therapy
- Behavioral Modification
- Activities of Daily living (ADL)-
- Self-care skills (feeding, dressing, grooming, etc.)
- Skills related to school performance (e.g.: printing, cutting, etc.)
- Play and leisure skills
- Fine Motor Activities.
A.D.H.D. (Attention-Deficit Hyperactivity Disorder)
Attention deficit hyperactivity disorder (ADHD) is a behavioral syndrome characterized by developmentally inappropriate levels of inattention or hyperactivity and impulsivity that interfere significantly with function.

There are three presentations of ADHD:
- Inattentive
- Hyperactive-impulsive
- Combined inattentive & hyperactive-impulsive
Cause:
- Traumatic brain injury.
- Alcohol and tobacco use during pregnancy.
- Low birth weight.
- Premature delivery.
- Chemical exposure.
- Family history.
- Eating too much sugar.
- Food additives.
- TV or video games.
HOW OCCUPATIONAL THERAPY CAN HELP?
- Remedial strategies aim to restore an impaired capacity such as, attention, problem solving skill etc.
- Sensory integration therapy
- Behavior Therapy
- Cognitive Behavioral Therapy(CBT)
- Adaptive strategies
- Social skills training
- Group therapy
- Perform the ADLs: The child can do the activities of daily living such as, brushing, grooming, bathing, toileting etc. by him/herself.
- Parenting skills training is for understanding and managing the child’s behaviors
Intellectual Disability
Tab Content
Hand Therapy
Tab Content
Mental Health
Tab Content
Inclusive School
Tab Content
C.B.R. (Community Based Rehabilitation)
Tab Content
Ergonomics
Tab Content
Splinting & Assistive Device
Tab Content
Physio Therapy
Occupational Therapy
Speech & Language Therapy

